The Research
A COLLECTION OF PERSONAL DECON STUDIES
This page includes a summary of select research studies and our interpretation as it relates to exposure and decontamination in the fire service. It is by no means an exhaustive list, but hopefully provides a helpful central location for what we believe to be key studies and their findings.
We encourage you to read and interpret each study on your own, continue your research outside of this source and adjust your decontamination protocol accordingly. Our purpose remains to be helpful in the development of decontamination protocol and to help reduce the risk of exposure.
Thank you for your interest in personal decontamination and firefighter health and wellness. We hope to become your partner in this mission to change the stats.
FIREFIGHTER EXPOSURE
The IARC Monographs: Firefighting Categorized as a Group 1 Carcinogen, 2022
In July of 2022, 25 scientists from 8 countries met at the World Health Organization’s (W.H.O.) International Agency for Research on Cancer (IARC) in Lyon, France, to review available research and finalize their decision on the carcinogenicity of firefighting as an occupation.
After more than a decade of research, the profession of firefighting has moved from a "Group 2B - Possibly carcinogenic to humans" categorization to a "Group 1 - Carcinogenic to Humans" (entirely skipping 2A - 'probably carcinogenic’).
Read the IARC release on Monograph 132 evaluating the carcinogenicity of occupational exposure as a firefighter.
Dermal Absorption of PAHs in Firefighters - Ottawa University, 2017
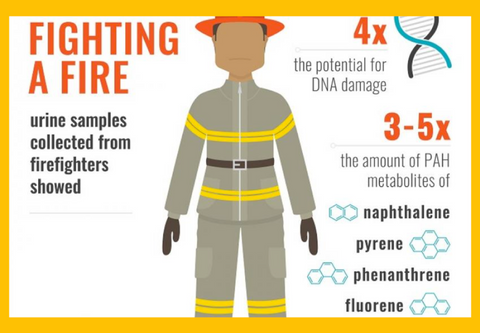
The University of Ottawa (J. Keir) studied PAH levels in firefighters by testing firefighters' urine before and after an incident. Results showed firefighters had 3-5x more PAH metabolites in their urine after a fire then before, giving 4x the potential for DNA damage.
This study proved toxins are absorbing through the skin, regardless of bunker gear protection.
Heavy areas of chemical concentration and absorption on the body included the:
- scalp
- head & face / jaw
- neck
- hands
- underarms
- groin area
Keir JLA, Akhtar US, Matschke DMJ, Kirkham TL, Chan HM, Ayotte P, White PA, Blais JM. Elevated Exposures to Polycyclic Aromatic Hydrocarbons and Other Organic Mutagens in Ottawa Firefighters Participating in Emergency, On-Shift Fire Suppression. Environ Sci Technol. 2017 Nov 7;51(21):12745-12755. doi: 10.1021/acs.est.7b02850. Epub 2017 Oct 18. PMID: 29043785.
The Science of Smell - Tucson AZ, 2021
Evaluation of fireground exposures using urinary PAH metabolites, 2021
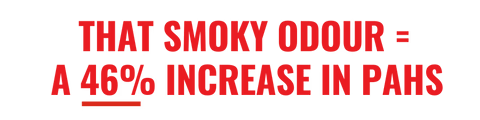
This 2021 study on 242 Tucson, AZ firefighters showed a direct correlation between that notoriously difficult-to-remove smoke odour left on your skin after a fire and a 46% increase in post-incident urinary Polycyclic Aromatic Hydrocarbons (PAH) levels, meaning that smoky odour left behind is “significantly” associated with an increase in PAH levels in your body. To translate, that smoky odour persisting even after you shower = a 46% increase in PAH toxins INSIDE your body.
If you're still smelling smoke after you shower, your soap isn't cutting it.
Hoppe-Jones C, Griffin SC, Gulotta JJ, Wallentine DD, Moore PK, Beitel SC, Flahr LM, Zhai J, Zhou JJ, Littau SR, Dearmon-Moore D, Jung AM, Garavito F, Snyder SA, Burgess JL. Evaluation of fireground exposures using urinary PAH metabolites. J Expo Sci Environ Epidemiol. 2021 Sep;31(5):913-922. doi: 10.1038/s41370-021-00311-x. Epub 2021 Mar 2. PMID: 33654270; PMCID: PMC8445814.
SURFACE TRANSFER
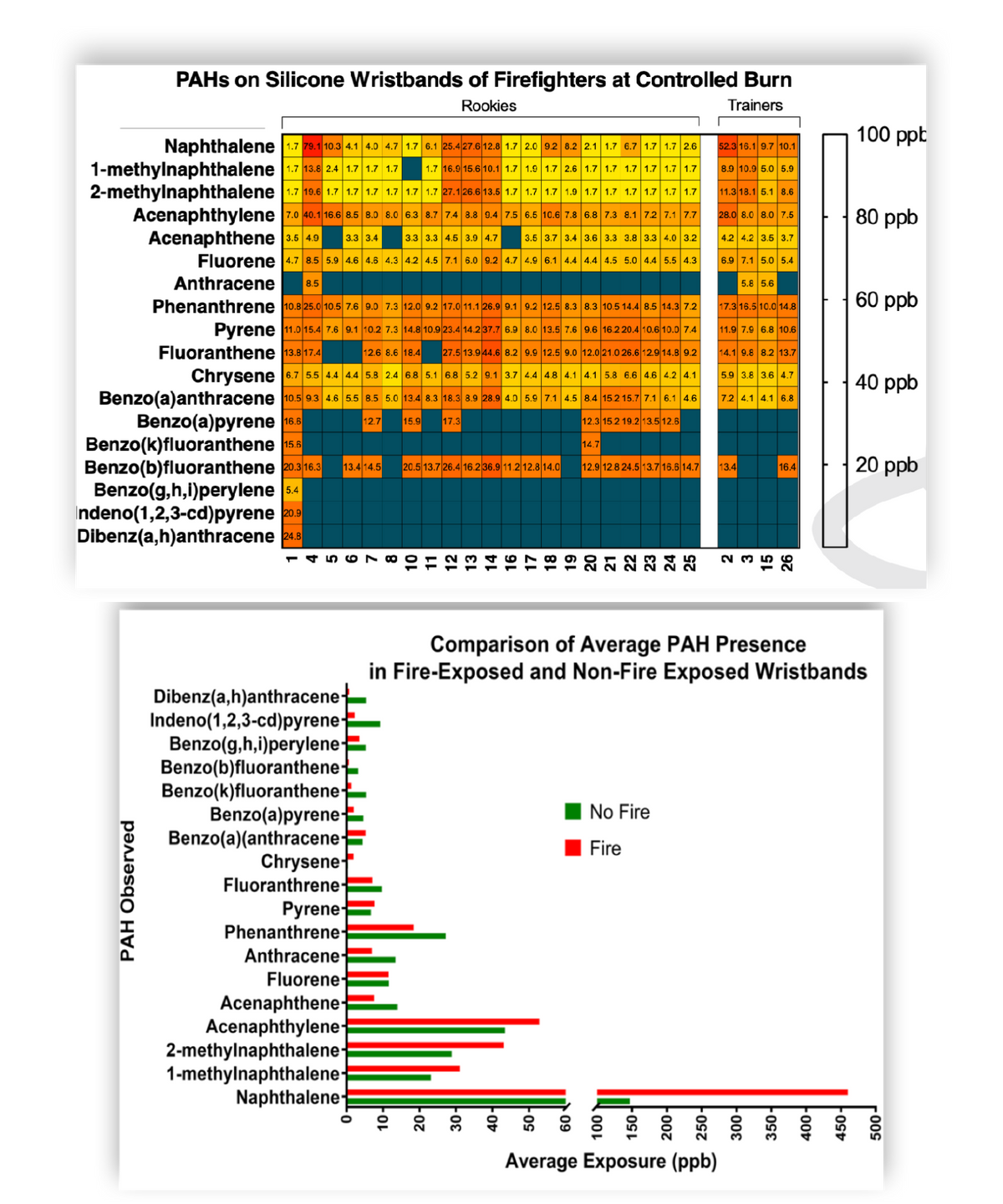
PAH Exposure of firefighters at a Controlled Burn - City of Miami Fire Rescue, 2020
Surface exposure, substance transfer, or ‘toxic handoff’ refers to exposure through physical transference. Toxins are easily picked up from one surface - or person - to another, depending on their volatility and prevalence. You can expose others as they transfer from your person to your clothing, equipment, vehicle … all the way home.
The City of Miami Fire Rescue used silicone wristbands to measure the presence of PAHs in firefighters both exposed to fire (a controlled burn), and those not exposed. In some cases, those not exposed to the fire had higher levels of PAHs than those who were exposed, most notably with the lower molecular weight (higher volatility) compounds, but still very much an issue across all PAHs measured, illustrating the danger of toxic handoff.
Evaluation of silicone-based wristbands as passive sampling systems using PAHs as an exposure proxy for carcinogen monitoring in firefighters: Evidence from the firefighter cancer initiative, 2020
The Invisible Danger of Bunker Gear Transfer [VIDEO] - City of Miami Sylvester Comprehensive Cancer Center, 2019
The University of Miami (Sylvester Comprehensive Cancer Centre) did an interesting experiment using glow-in-the-dark powder to mimic soot in an effort to illustrate secondary and tertiary transfer, tracking soot (toxins) from an incident all the way to a child’s soccer ball.
This video demonstrates processes of cross-contamination from bunker gear to individuals, equipment, the fire station, personal vehicles, and even family members. This video has been evaluated and has been shown to be effective at increasing intentions to engage in decontamination processes after a fire, including showering, routine cleaning of gear, bagging gear before transport, and using wipes on scene.
Remember - 97% of particulates to which you are exposed cannot be seen, meaning the soot you do see only accounts for 3% of your exposure.

Cancer Rates in Children of Firefighters - Kitsap County, WA, 2020
This applied research project in Kitsap County, Washington determined children of firefighters were 27.4 TIMES more likely to be diagnosed with cancer than the general population.
The chance of diagnosis among general child population was found to be 0.0179%, whereas the child of a Kitsap County firefighter has a 0.49% chance of being diagnosed with cancer.
Ronald E. Powers, South Kitsap Fire Rescue, Port Orchard Washington, 2020
DECONTAMINATION
Methods of Decontamination and Effectiveness on Bunker Gear - collection of studies
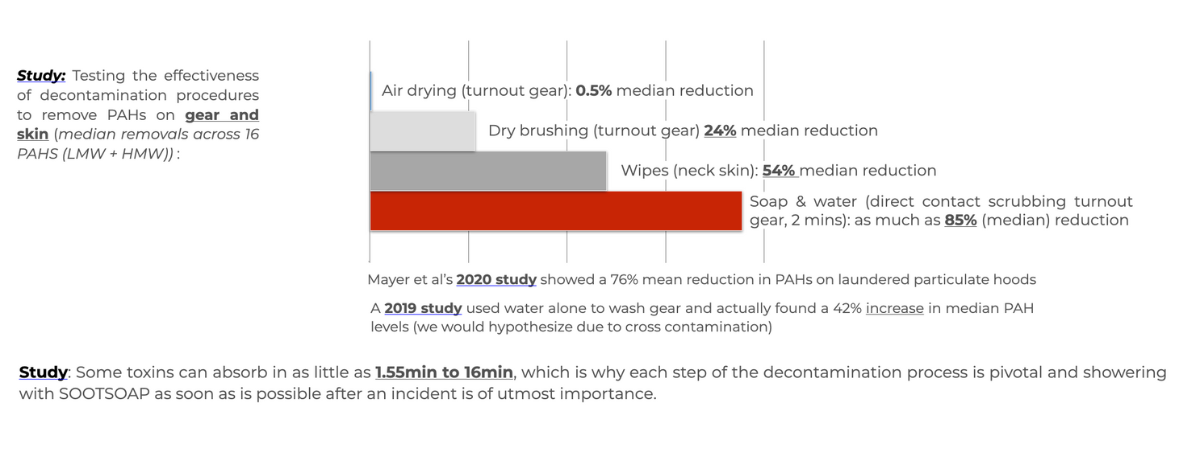
Wet Decon with soap and water is the most effective way of removing toxins and a pivotal part of the decon process. Wipes have been shown to remove up to 54% from those areas they can get to at an incident and, though we haven't seen a study on this to date, we imagine these %s are much less for areas with hair including the head/scalp, underarms and groin area, not to mention the parts of the body that aren't engaged by a wipe at all.
Air drying showed a 0.5% median reduction, dry brushing turnout gear showed a 24% median reduction, and direct-contact scrubbing with soap and water for 2 minutes showed 85% reduction (Forsberg study (2020), though we know this to be closer to 36% with average laundering procedures (Fent, 2017). The researchers at NIOSH have divulged to us they have not seen decontamination numbers higher than 40% on bunker gear when laundered.
This means that 60%+ of toxins from the previous incident remain on bunker gear even after it's been laundered.
Further, some toxins can absorb in as little as 1.55min to 16min (Keir), which is why each step of the decontamination process is pivotal and showering with a proven decontaminating soap as soon as is possible after an incident is of utmost importance.
Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures, 2017
Fent KW, Alexander B, Roberts J, Robertson S, Toennis C, Sammons D, Bertke S, Kerber S, Smith D, Horn G. Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures. J Occup Environ Hyg. 2017 Oct;14(10):801-814. doi: 10.1080/15459624.2017.1334904. PMID: 28636458.
Decontamination efficacy of soapy water and water washing following exposure of toxic chemicals on human skin, 2020
Emma Forsberg, Linda Öberg, Elisabet Artursson, Elisabeth Wigenstam, Anders Bucht & Lina Thors (2020) Decontamination efficacy of soapy water and water washing following exposure of toxic chemicals on human skin, Cutaneous and Ocular Toxicology, 39:2, 134-142, DOI: 10.1080/15569527.2020.1748046
Effectiveness of dermal cleaning interventions for reducing firefighters’ exposures to PAHs and genotoxins, 2023
Jennifer L. A. Keir, Tracy L. Kirkham, Rocio Aranda-Rodriguez, Paul A. White & Jules M. Blais (2023) Effectiveness of dermal cleaning interventions for reducing firefighters’ exposures to PAHs and genotoxins, Journal of Occupational and Environmental Hygiene, 20:2, 84-94, DOI: 10.1080/15459624.2022.2150768
Air drying showed a 0.5% median reduction, dry brushing turnout gear showed a 24% median reduction, and direct-contact scrubbing with soap and water for 2 minutes showed 85% reduction (Forsberg study (2020), though we know this to be closer to 36% with average laundering procedures (Fent, 2017). The researchers at NIOSH have divulged to us they have not seen decontamination numbers higher than 40% on bunker gear when laundered.
This means that 60%+ of toxins from the previous incident remain on bunker gear even after it's been laundered.
Further, some toxins can absorb in as little as 1.55min to 16min (Keir), which is why each step of the decontamination process is pivotal and showering with a proven decontaminating soap as soon as is possible after an incident is of utmost importance.
SOOTSOAP and the Removal of PAHs - NC State University, 2023
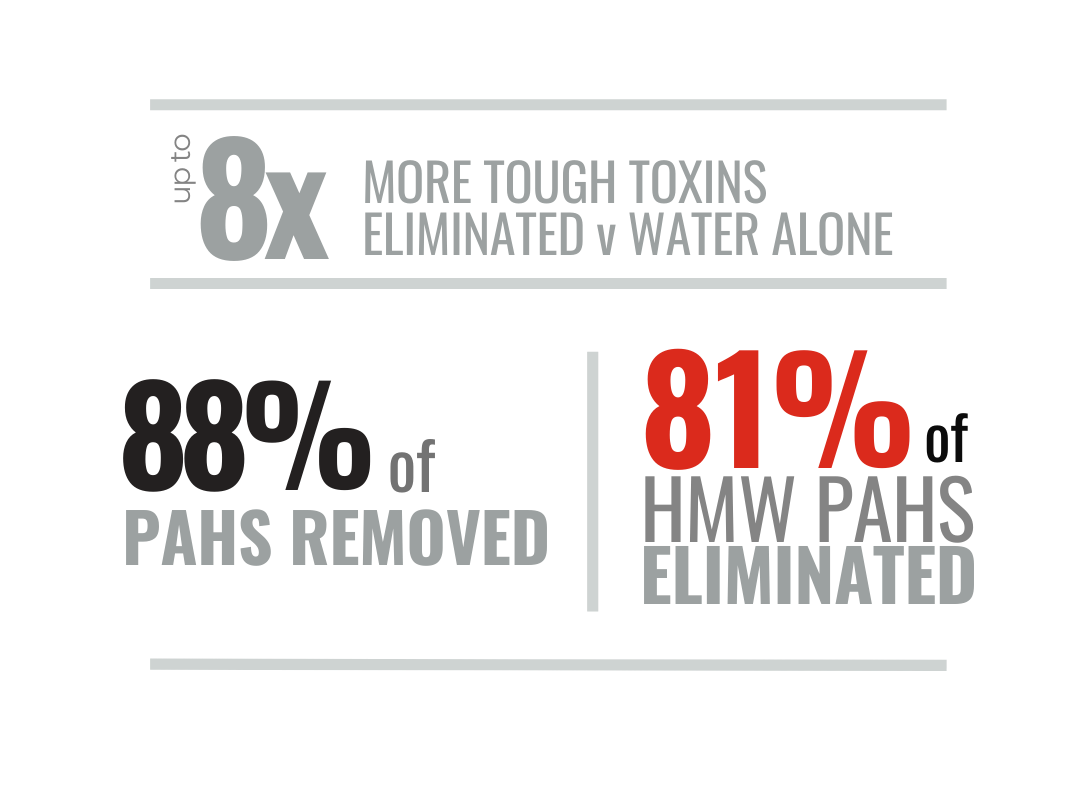
North Carolina State University's Wilson College of Textiles recently evaluated SOOTSOAP's performance in the removal of PAHs, as well as the effectiveness of 3 other personal decontamination products.
SOOTSOAP was found to remove up to 8x more PAHs than water alone, with an average efficacy of 87.8% median removal, particularly effective targeting the more difficult-to remove HMW PAHs with an average of 81% efficacy - notably higher than any other personal decon product tested.
Download our pamphlet further explaining this research as it relates to personal decontamination.
Hossain MT, Girase AG, Ormond RB. Evaluating the performance of surfactant and charcoal-based cleaning products to effectively remove PAHs from firefighter gear. Front Mater. 2023 May 11;10(May):10.3389/fmats.2023.1142777. doi: 10.3389/fmats.2023.1142777. PMID: 38073671; PMCID: PMC10698686. https://pubmed.ncbi.nlm.nih.gov/38073671/